The treatment of chronic lymphocytic leukemia (CLL) has been radically changed in the last years thanks to the targeted therapies, including kinase (i.e. ibrutinib) and BCL2 (i.e. venetoclax) inhibitors. Venetoclax (VEN) in particular is able to obtain undetectable minimal residual disease (uMRD), though only in a proportion of patients (pts) when given as single agent, thus warranting the need of different strategies in those not achieving uMRD.
We designed a phase 2 multicenter Italian study where ibrutinib (IBR) is added to VEN based on a MRD-driven strategy aiming at obtaining uMRD and discontinuing both treatments in pts who did not achieve uMRD with VEN mono.
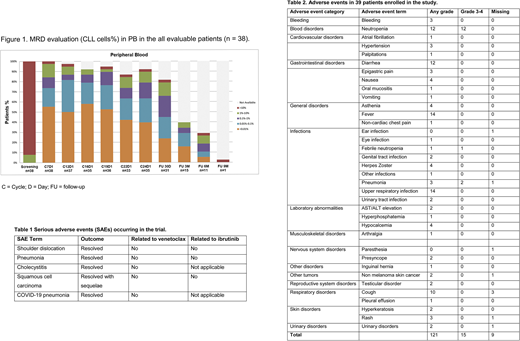
Study treatment started with VEN (ramp up to 400 mg/day as per current label) for 12 months. MRD status in peripheral blood (PB) and bone marrow (BM) was evaluated using the 6-color flow cytometry assay recommended by ERIC (CD5/CD81/CD79b/CD19/CD43/CD20). Pts with uMRD in both PB and BM at C12D1 discontinued VEN at C12D28 and entered the follow-up phase. Pts with detectable MRD in PB and/or BM added IBR 420 mg/day starting from C13D1 and continued both drugs up to maximum C24D28, uMRD, progression or unacceptable toxicity (whichever occurs first). After C24D28, pts with detectable MRD and still in response continued IBR alone. The primary endpoint was uMRD4 (<1 CLL cell in 104 leukocytes) in both PB and BM. We report here the results as of 15Jul2020 (data cutoff).
Thirty-eight pts (recruited from Nov 2017 to Jul 2018) fulfilled eligibility and started VEN. Baseline characteristics included: median number of prior therapies 1 (range 1-4) (60.6% previously treated with FCR or FC); del(17p) in 8/33 (24%); TP53 mutations in 10/30 (33%), and unmutated IGHV in 24/30 (80%). At the data cut-off, 35/38 evaluable pts still in the study have reached C24D1, 1 pt discontinued treatment due to myelodisplasia (considered unrelated to study treatment) before C12D1 and 1 pt progressed on VEN monotherapy shortly before that timepoint, 1 evaluation is still missing due to COVID-19 restrictions.
At C12D1, uMRD4 in PB was achieved in 19/38 (50%) pts (Figure 1), 17/19 (89.5%) had uMRD4 confirmed in BM. Overall response rate with VEN single-agent was 36/38 (94.7%), 9 CR and 27 PR. As per protocol, the 17 pts (45%) with uMRD4 in PB and BM at C12D1 discontinued VEN at C12D28. Nineteen responsive cases with detectable MRD at C12D1 added IBR to VEN starting from C13D1. The combination of IBR and VEN led to an improved reduction of the depth of MRD in all but 3 pts with 16/19 (84%) achieving uMRD4 in both PB and BM between C16D1 (first MRD assessment after starting IBR) and C24D1, thus stopping both therapies as per protocol. After a median follow-up of 25.4 months (range 6.1-33.5) from treatment initiation, no clinical progression was observed among those discontinuing treatment in uMRD, while MRD4 relapse occurred in 21/33. Median time to MRD4 relapse in those who achieved uMRD at any timepoint and discontinued treatment was 4 months (range 2-13). Twelve pts (6 treated with VEN only) remain uMRD after stopping treatment, with a median observation of 13 months (range 3+-18+) since confirmed uMRD4.
Safety data were analyzed in the intention-to-treat cohort (39 pts). No cases of clinical tumor lysis syndrome (TLS) and/or biochemical TLS were reported in the 39 pts exposed to VEN. Adverse events (AEs) were mild, with no treatment discontinuations or dose reductions.
Five Serious AEs (Table 1) and 130 AEs (Table 2) occurred in 28 patients, without any SUSARs. All 5 SAEs were deemed unrelated to study drug(s) and 4/5 have resolved without sequelae.
In conclusion, we here present the updated results of our study including the combination phase of VEN with IBR. This sequential MRD-guided approach was feasible and led to deeper responses in about 85% of pts not achieving uMRD4 after VEN alone. With this tailored and time-limited strategy 33 out of 38 pts (87%) obtained uMRD4 in PB and BM either after VEN monotherapy or the IBR-VEN combination, indicating we may reach identical depth of response with a personalized intensification and avoid unnecessary drug exposure. Time to clinical progression and response to VEN retreatment in this cohort remain to be established as well as the biological characteristics of those pts with persistent MRD despite the combined treatment. Updated results with further sequential MRD and clinical monitoring after treatment discontinuation will be presented at the meeting.
Scarfo:Gilead: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Honoraria; Abbvie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Farina:Abbvie: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees. Gaidano:Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Astrazeneca: Membership on an entity's Board of Directors or advisory committees; Sunesys: Membership on an entity's Board of Directors or advisory committees. Reda:Janssen: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees. Coscia:Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Shire: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Karyopharm Therapeutics: Research Funding. Laurenti:Roche: Honoraria; Gilead: Honoraria; Janssen: Honoraria; AbbVie: Honoraria. Varettoni:Roche: Consultancy, Membership on an entity's Board of Directors or advisory committees; AbbVie: Other: Travel/accommodations/expenses; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel/accommodations/expenses. Ghia:Lilly: Consultancy, Honoraria; Sunesis: Consultancy, Honoraria, Research Funding; Adaptive, Dynamo: Consultancy, Honoraria; MEI: Consultancy, Honoraria; Celgene/Juno: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding; BeiGene: Consultancy, Honoraria; Acerta/AstraZeneca: Consultancy, Honoraria; ArQule: Consultancy, Honoraria; Gilead: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal